Question: Case 4-2014: A 39-Year-Old Man With Night Sweats And Abdominal Pain Daniel P. Hunt, M.D., Victorine V. Muse, M.D., And Amy Ly, M.D. PRESENTATION OF CASE Dr. Jordan B. Strom (Medicine): A 39-year-old Man Was Admitted To This Hospital Be- From The Departments Of Medicine Cause Of Night Sweats And Abdominal Pain. (D.P.H.), Radiology (V.V.M.), And Pathol. …
I need a full summary for this article please with fullyexplained sentences.
Transcribed Image Text from this Question
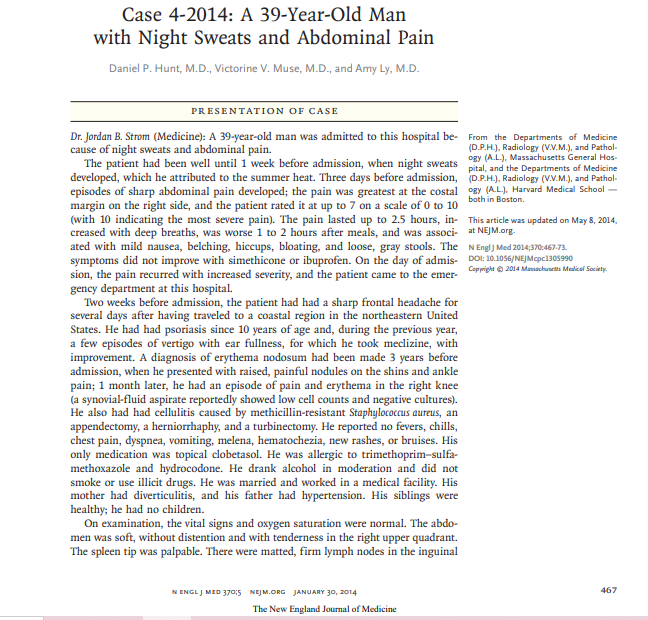
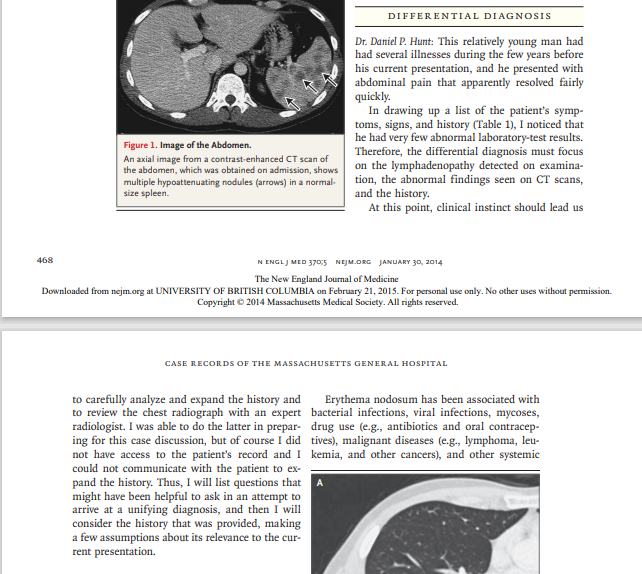
Case 4-2014: A 39-Year-Old Man with Night Sweats and Abdominal Pain Daniel P. Hunt, M.D., Victorine V. Muse, M.D., and Amy Ly, M.D. PRESENTATION OF CASE Dr. Jordan B. Strom (Medicine): A 39-year-old man was admitted to this hospital be- from the Departments of Medicine cause of night sweats and abdominal pain. (D.P.H.), Radiology (V.V.M.), and Pathol. The patient had been well until 1 week before admission, when night sweats pital , and the Departments of Medicine ogy (A.L.), Massachusetts General Hos. developed, which he attributed to the summer heat. Three days before admission, D.P.H.), Radiology (V.V.M.), and Pathol. episodes of sharp abdominal pain developed, the pain was greatest at the costal psy (A.L.), Harvard Medical School – both in Boston. margin on the right side, and the patient rated it at up to 7 on a scale of 0 to 10 (with 10 indicating the most severe pain). The pain lasted up to 2.5 hours, in- This article was updated on May 8, 2014, creased with deep breaths, was worse 1 to 2 hours after meals, and was associat NEJM.org. ated with mild nausea, belching, hiccups, bloating, and loose, gray stools. The N Engl] Med 2014,370-467-73. symptoms did not improve with simethicone or ibuprofen. On the day of admis. DOI: 10.1056/NEJMcpc1305990 sion, the pain recurred with increased severity, and the patient came to the emer- Copright © 2014 danachusetts Metal Society. gency department at this hospital. Two weeks before admission, the patient had had a sharp frontal headache for several days after having traveled to a coastal region in the northeastern United States. He had had psoriasis since 10 years of age and, during the previous year, a few episodes of vertigo with ear fullness, for which he took meclizine, with improvement. A diagnosis of erythema nodosum had been made 3 years before admission, when he presented with raised, painful nodules on the shins and ankle pain; 1 month later, he had an episode of pain and erythema in the right knee (a synovial-fluid aspirate reportedly showed low cell counts and negative cultures). He also had had cellulitis caused by methicillin-resistant Staphylococcus aureus, an appendectomy, a herniorrhaphy, and a turbinectomy. He reported no fevers, chills, chest pain, dyspnea, vomiting, melena, hematochezia, new rashes, or bruises. His only medication was topical clobetasol. He was allergic to trimethoprim-sulfa- methoxazole and hydrocodone. He drank alcohol in moderation and did not smoke or use illicit drugs. He was married and worked in a medical facility. His mother had diverticulitis, and his father had hypertension. His siblings were healthy; he had no children. On examination, the vital signs and oxygen saturation were normal. The abdo- men was soft, without distention and with tenderness in the right upper quadrant The spleen tip was palpable. There were matted, firm lymph nodes in the inguinal 467 N ENGL J MED 370:5 NEJM.ORG JANUARY 30, 2014 The New England Journal of Medicine region and hyperpigmented, scaly plaques on after the administration of contrast material, the lower legs and waist; the remainder of the showed numerous ill-defined, hypoattenuating examination was normal. The white-cell countlesions, 1 to 2 cm in diameter, in the spleen was 5800 per cubic millimeter (reference range, (Fig. 1), as well as bilateral, dependent atelectasis 4500 to 11,000), with 73% neutrophils (refer- in the lungs. A hypoattenuating lesion in the ence range, 40 to 70), 14% lymphocytes (refer- liver, measuring less than 1 cm in diameter, was ence range, 22 to 44), 6% monocytes (reference slightly increased in size from a study 8 years range, 4 to 11), and 7% eosinophils (reference earlier and was thought to represent a cyst; range, 0 to 8); the blood level of C-reactive pro- small, nonspecific retroperitoneal and mesen- tein was 9.7 mg per liter (reference range, <8.0, teric lymph nodes were also seen. A chest radio- negative for inflammation), and the blood level graph showed an ill-defined opacity in the left of angiotensin-converting enzyme (ACE) was 55 U apex, overlying the end of the first rib, and a per liter (reference range, 8 to 53). The remain-rounded opacity in the left hilar region. An ul- der of the complete blood count, the erythrocyte trasound examination of the legs revealed be- sedimentation rate, and a urinalysis were nor nign-appearing enlarged inguinal lymph nodes, mal, as were results of coagulation and renal- and the largest of which was 1.5 cm by 0.6 cm. liver-function tests and blood levels of electro- Dr. Strom: The patient’s abdominal pain im- lytes, calcium, phosphorus, magnesium, glu- proved, and he was discharged on the second cose, lactate dehydrogenase, amylase, and li- hospital day. pase. Testing for human immunodeficiency Dr. Muse: At a follow-up visit 2 days after dis- virus types 1 and 2, hepatitis C virus antibodies, charge, a CT scan of the chest, obtained after and hepatitis B virus surface antigen was nega- the administration of contrast material, showed tive; testing for hepatitis B virus surface anti mediastinal lymphadenopathy, with lymph nodes bodies was positive. An electrocardiogram (ECG) as large as 1.8 cm in diameter. The CT scan also showed normal sinus rhythm, with a borderline showed bilateral hilar lymphadenopathy, an en- early-repolarization abnormality and T-wave in- larged anterior diaphragmatic lymph node (1.2 cm versions in leads V, and V.. Ultrasonography of in diameter), clustered nodular opacities within the abdomen revealed multiple rounded, hy. the lung in a perilymphatic distribution (Fig. 2), poechoic areas in the spleen, which was not multiple splenic lesions, a hypervascular lesion enlarged, with no evidence of cholelithiasis or in the posterior right lobe of the liver, and a cholecystitis. The patient was admitted to the hypodense lesion (0.6 cm in diameter) in the left hospital. lobe of the liver, which was thought to represent Dr. Victorine V. Muse: Computed tomographic a hepatic cyst. (CT) scans of the abdomen and pelvis, obtained Dr. Strom: Several days later, a diagnostic test was performed. DIFFERENTIAL DIAGNOSIS Dr. Daniel P. Hunt: This relatively young man had had several illnesses during the few years before his current presentation, and he presented with abdominal pain that apparently resolved fairly quickly. In drawing up a list of the patient’s symp- toms, signs, and history (Table 1), I noticed that he had very few abnormal laboratory-test results. Therefore, the differential diagnosis must focus on the lymphadenopathy detected on examina- tion, the abnormal findings seen on CT scans, and the history. At this point, clinical instinct should lead us Figure 1. Image of the Abdomen. An axial image from a contrast-enhanced CT scan of the abdomen, which was obtained on admission, shows multiple hypoattenuating nodules (arrows) in a normal size spleen. 468 N ENGL J MED 3705 NEJM.ORG JANUARY 30, 2014 The New England Journal of Medicine Downloaded from nejm.org at UNIVERSITY OF BRITISH COLUMBIA on February 21, 2015. For personal use only. No other uses without permission. Copyright © 2014 Massachusetts Medical Society. All rights reserved. CASE RECORDS OF THE MASSACHUSETTS GENERAL HOSPITAL to carefully analyze and expand the history and Erythema nodosum has been associated with to review the chest radiograph with an expert bacterial infections, viral infections, mycoses, radiologist. I was able to do the latter in prepar- drug use (e.g., antibiotics and oral contracep- ing for this case discussion, but of course I did tives), malignant diseases (e.g., lymphoma, leu- not have access to the patient’s record and I kemia, and other cancers), and other systemic could not communicate with the patient to ex- pand the history. Thus, I will list questions that might have been helpful to ask in an attempt to arrive at a unifying diagnosis, and then I will consider the history that was provided, making a few assumptions about its relevance to the cur- rent presentation. PSORIASIS We need to ask a few questions about this pa- tient’s history of psoriasis. What was the extent of involvement? Had there been joint involve- ment? How had the illness progressed over the years? Which treatments had he received? Had he received biologic agents? How did the psoriasis affect his life? We should ask these questions to estimate the potential for illnesses associated with psoriasis or long-term consequences. Asso- ciated illnesses include psoriatic arthritis, car- diovascular disease, depression, anxiety, non- melanoma skin cancer, and lymphoma.” I am particularly concerned about lymphoma in this patient with widespread lymphadenopathy and abnormal findings in the spleen, because a num- ber of studies suggest that patients with psoriasis have an increased risk of lymphoma 2-4 Because of the potential association between psoriasis and lymphoma, we need to include lymphoma in our differential diagnosis. ERYTHEMA NODOSUM Next, we should investigate the patient’s history of erythema nodosum. At the time of the epi- sode, was another diagnosis made? How long did the episode last? Were there other symptoms? Did he receive any treatment? Was a chest radio- graph obtained? In fact, when I reviewed the radiology report for this case with Dr. Muse, it became apparent that a radiograph had been ob- tained as part of the evaluation for erythema no- dosum and showed a right hilar fullness and a right paratracheal density, features possibly con- Figure 2. Images of the Chest. A CT scan of the lung shows bilateral peribronchovas sistent with lymphadenopathy. The potential cular nodules (Panel A, arrows), with a cluster in the presence of lymphadenopathy at least 3 years ear- left upper lobe (Panel B, arrow). Subcarinal lymphade lier was reassuring and led me to feel more cer- nopathy was also seen (Panel C, arrow). tain about the diagnosis in this case. N ENGL) MED 370,5 NEJM.ORG JANUARY 30, 2014 469 The New England Journal of Medicine Downloaded from neimare at UNIVERSITY OF BRITISH COLUMBIA on February 21 2015 For pronal en olv No others without nermission The NEW ENGLAND JOURNAL OF MEDICINE raise the possibility of a diagnosis of Löfgren’s Table 1. Symptoms, Signs, and History, syndrome, although the presence of hilar lymph- Symptoms adenopathy is generally also required for this di- Abdominal pain on the right side with a pleuritic.com agnosis. Löfgren’s syndrome is a form of sarcoid- ponent osis that is characterized by the triad of erythema Night sweats during the past week nodosum, arthralgias, and hilar lymphadenopa- Recent frontal headache apparently resolved thy, it is usually self-limited, although its mani- Signs festations may persist for several years. A small Palpable spleen tip number of patients with Löfgren’s syndrome have Hypoattenuating splenic lesions on CT normal chest radiographs at the time of diagno- sis; most patients have hilar lymphadenopathy, Matted, firminguinal lymph nodes 13% of patients have respiratory symptoms, and Bilateral hilar lymphadenopathy on chest CT 4% of patients have peripheral lymphadenopa- White-cell count of 5800, with 14% lymphocytes thay? Furthermore, 6% of patients have a recur Minimally elevated blood level of Creative protein rence of sarcoidosis within 18 months to 20 years (9.7 mg/liter) after presenting with Löfgren’s syndrome. I think Minimally elevated blood level of angiotensin-convert the episode of erythema nodosum, the ankle ing enzyme (55 Uiter) pain, and the knee arthritis were manifestations Positive test for hepatitis B virus surface antibodies of Löfgren’s syndrome, in which case, sarcoid- (probably due to immunization) osis would be the leading potential diagnosis. T-wave inversions in the inferior leads on ECG Does sarcoidosis account for the other features of this patient’s presentation (Table 112 Gastroin- Psoriasis since 10 years of age testinal manifestations of sarcoidosis primarily Intermittent vertigo with ear fullness during the past involve the stomach, and patients can present with abdominal pain, nausea, vomiting, and Episode of erythema nodosium 3 years previously weight loss. Headaches, such as the one this Previous cellulitis caused by methicillin-resistant patient reportedly had during the weeks before Staphylococcus aureus admission, are sometimes a manifestation of Previous appendectomy, herniorraphy, and turbi sarcoidosis. The patient’s hypoattenuating splen- nectomy is lesions are consistent with sarcoidosis. Are the findings on this patient’s chest imag- ing consistent with sarcoidosis? Approximately diseases (e.g., sarcoidosis, enteropathies, Sweet’s 85% of patients with sarcoidosis have intratho- syndrome, and Takayasu’s disease). Many dis- racic lymphadenopathy, typically bilateral hilar eases are associated with erythema nodosum, and right paratracheal lymphadenopathy.” When and among patients in whom a cause of erythe- I reviewed the radiograph before this conference, ma nodosum is identified, streptococcal infec. I was impressed by the predominance of the find- tion and sarcoidosis are fairly common diagno- ings in the upper lung and the coexistent medi- ses. However, in most patients, an underlying astinal lymphadenopathy, features that suggest diagnosis is not made. On the basis of this sarcoidosis. Given the findings on the chestra patient’s history, streptococcal infection seems diograph in this case, I strongly suspect that the unlikely. However, the presence of lymphade diagnosis is sarcoidosis, although there are still nopathy and the history of erythema nodosum a few issues to address may point toward a diagnosis of sarcoidosis. We still need to consider the minimally ele- vated blood level of ACE. When the ACE level is SARCOIDOSIS AND LOFGREN’S STNDROME less than 25 U per liter, the likelihood ratio for When erythema nodosum developed in this pa sarcoidosis is 0.12, when the ACE level is be- tient, he also had ankle pain and within a tween 25 and 71 U per liter, the likelihood ratio month, an episode of arthritis of the right knee is 1.31; and when the ACE level is greater than that prompted joint aspiration. The combination 71 per liter, the likelihood ratio increases to of erythema nodosum and ankle pain should 7.15.42 This patient had an ACE level of 55 U per