Paper Details: three different models for combining vertical and horizontal integration in the UK
Practice-based commissioning (PBC) in the UK is intended to improve both the vertical and horizontal integration of health care, in order to avoid escalating costs and enhance population health. Vertical integration involves patient pathways to treat named medical conditions that transcend organizational boundaries and connect community-based generalists with largely hospital-sited specialists, whereas horizontal integration involves peer-based and cross-sectoral collaboration to improve overall health. Effective mechanisms are now needed to permit ongoing dialogue between the vertical and horizontal dimensions to ensure that medical and nonmedical care are both used to their best advantage. This paper proposes three different models for combining vertical and horizontal integration – each is a hybrid of internationally recognized ideal types of primary care organization. Leaders of PBC should consider a range of models and apply them in ways that are relevant to the local context. General practitioners, policymakers and others whose job it is to facilitate horizontal and vertical integration must learn to lead such combined approaches to integration if the UK is to avoid the mistakes of the USA in over-medicalizing health issues.
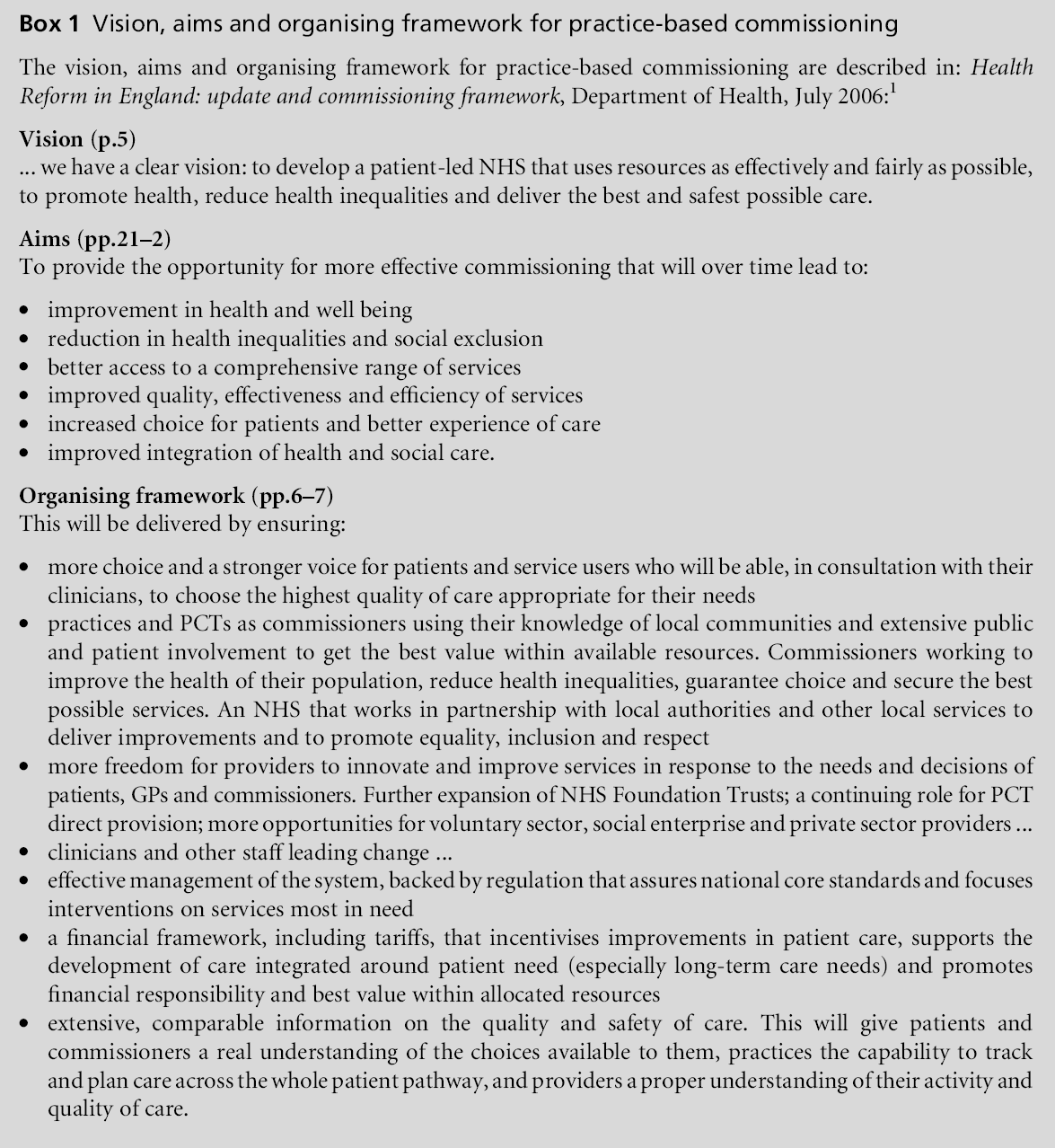
Practice-based commissioning (PBC) in the UK National Health Service (NHS) is an attempt to plan the best possible health care for entire populations (see Box 1).1 PBC will provide a local planning facility, led by general practitioners (GPs), to complement the systems-wide perspective of primary care trusts (PCTs). Together they will administer NHS funds for the population served.2
In order to plan best care, PBC must enable comprehensive integration of healthcare effort. Vertical integration involves patient pathways to treat named medical conditions, connecting generalists and specialists, whereas horizontal integration involves broadbased collaboration to improve overall health.3 Comprehensive integration includes a good balance of both.
Box 2 summarises the features of these two different types of integration. Broadly speaking, in terms of its data sources and status, vertical integration is the domain of medicine – diseases are researched as discrete entities; linear care pathways consider one disease at a time; discrete treatment packages are costed and evaluated for their anticipated effects; quality assurance emphasises achievement of quantifiable outcome targets. Broadly speaking, horizontal integration is the domain of social sciences – multidisciplinary teams and interagency collaboratives learn, inquire and innovate together; cross-organisational planning leads to a synchrony of effort that creates environments for health; quality assurance emphasisesmechanisms whereby broad groups of stakeholders can examine whole systems of care for their diffuse and unexpected long-term effects and then act for co-ordinated quality improvements.